Iron overload: too much of a good thing
Just like Goldilocks, our bodies like things to be ‘just right’. So, while it’s true that iron is essential for the human body to function properly, too much of a good thing can be harmful. Unfortunately, excess iron doesn’t equate to excess energy; in fact, it’s often quite the opposite.
Haemochromatosis—also known as inherited iron overload—is a condition that causes the body to absorb and store excess amounts of iron. It’s one of the most common genetic disorders in Australia, affecting around 1 in every 200 people of Northern European descent.
Sufferers may experience a range of symptoms, including fatigue, joint pain, weakness, weight loss and abdominal pain. Over time, the excess iron accumulates in specific areas of the body, eventually causing damage to tissues and organs, including the liver and heart. This can result in complications such as liver disease (cirrhosis), liver cancer, heart failure, diabetes, pigmented skin, arthritis, early menopause and impotence. If left undiagnosed, haemochromatosis can be fatal.
The good news is that early diagnosis, intervention and treatment can prevent further complications and allow a patient to live a normal life.

Type 1 haemochromatosis is hereditary, so if you have the condition you can thank your parents. Although haemochromatosis can be caused by faults in a range of different genes, most people with the condition have mutations in the HFE gene. The name HFE comes from ‘high iron’ (Fe being the chemical symbol for iron).
A properly functioning HFE gene basically helps to detect and regulate the amount of iron in the body. This means that for most of us, no matter how much meat, tofu or seafood we eat, our body will only take in as much iron as it needs.
If the HFE gene is faulty, however, our bodies begin to have an ‘all you can absorb’ iron party.
Symptoms, diagnosis and treatment
Haemochromatosis sounds like it should be easy to diagnose, but the problem is its general symptoms are relatively common health complaints—tiredness, abdominal pain, joint pain, and weakness.
The disorder is generally diagnosed in people over 40 because it takes time for iron levels in the body to accumulate. Women may be diagnosed later in life due to blood loss during child-bearing years (through menstruation and childbirth), which removes iron from the body. Younger people may have the condition but have not yet experienced any adverse symptoms. Each patient will also have their own unique level at which they may begin to feel the effects of iron overload. Because haemochromatosis is hereditary, it helps to know your family health history and talk about it with relatives.
A simple blood test can confirm haemochromatosis and, if discovered early, treatment is relatively simple and easy. The aim is to restore and then maintain safe iron levels in the body.
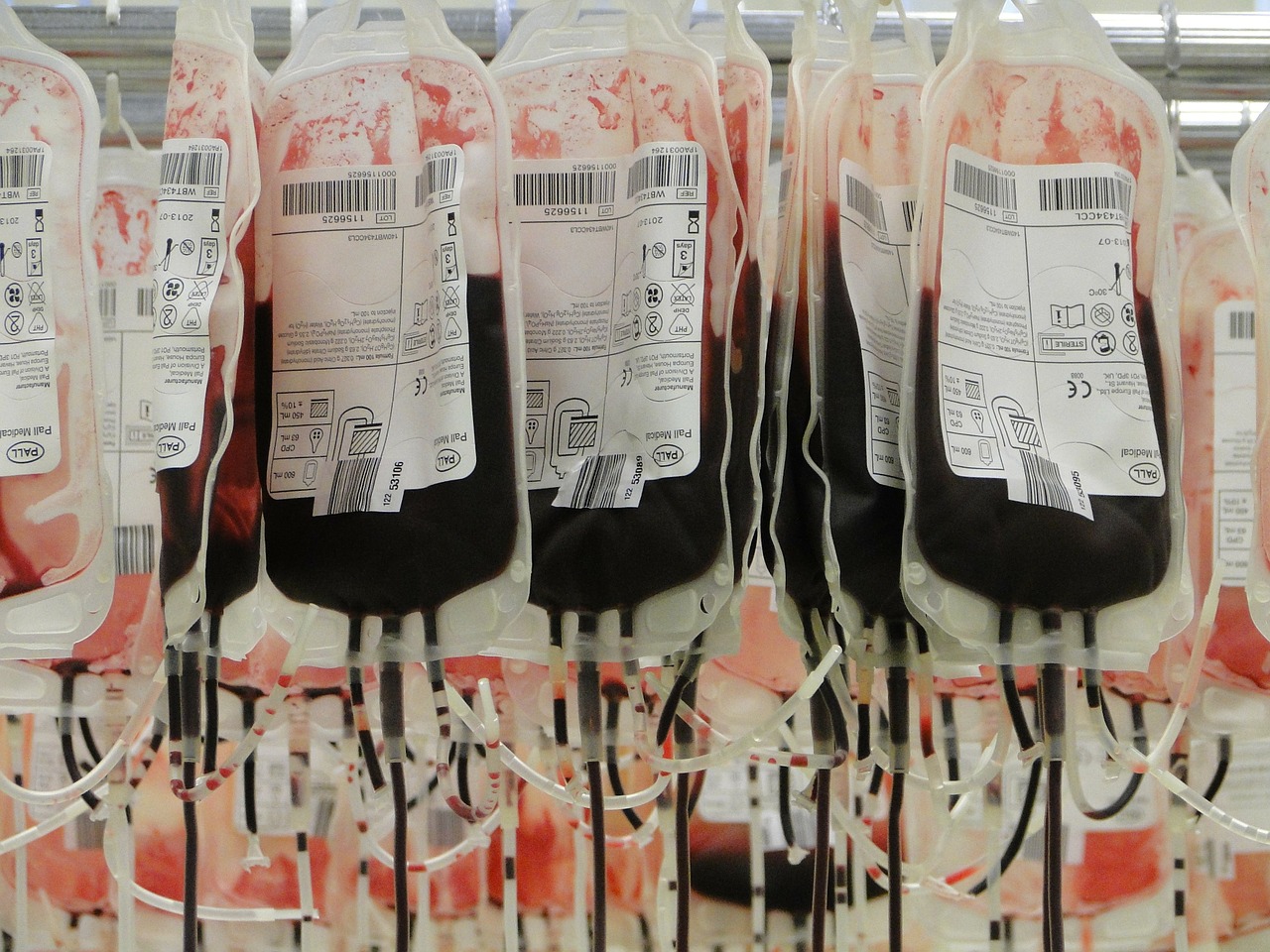
The most common form of treatment is venesection—the removal of between 300 mL and 500 mL of blood (similar to a blood donation) via a needle in the arm. This method has been used successfully since the 1940s and is safe, effective and low cost. Since haemochromatosis is not a blood disease, this blood can be safely transfused into other people (a win–win scenario), as long as there are no other reasons to prevent that person donating blood.
The reason venesection works is because once blood is removed from your system, some of the excess iron that is being stored by your body moves out of storage and is used to make new red blood cells.
Those few people who, for various reasons, cannot tolerate venesection therapy can be given drugs known as ‘iron chelators’. These are specially formulated to bind to iron so that it can be excreted from the body via urine.
Although haemochromatosis has the potential to be a serious health issue, the good news is that, if detected early, patients can lead a full and healthy life. An awareness and understanding of the symptoms, knowing your family’s medical history and annual check-ups with your GP can help to identify the condition early and manage it accordingly.






