COVID-19 vaccines and their long-term safety
8 November 2021
Getting vaccinated is one of the best things we can do to protect ourselves and our community against the worst of COVID-19. We’ve seen this in the vaccine rollout across the globe as those who are fully vaccinated are much less likely to die or suffer severe COVID-19. While there is an extremely rare risk of serious adverse reactions in the short term, the health risks of not getting the vaccine are much higher.
When considering the benefits of getting vaccinated, you may have wondered how we can be confident in the long-term safety of COVID-19 vaccines, especially the newer mRNA vaccines, that were developed recently. Experiences from previous vaccination programs and evidence about the current vaccines give scientists and regulators confidence that the vaccines approved for use in Australia are very unlikely to cause harm in the long term. In this article, we’ll take a look at why they can be confident in the long-term safety.

In Australia there are currently three COVID-19 vaccines provisionally approved for use: the Pfizer/BioNTech vaccine (Comirnaty), the AstraZeneca vaccine (Vaxzevria) and most recently, the Moderna vaccine (Spikevax). They have all passed the rigorous checks and balances required by the Therapeutic Goods Administration (TGA). To do so, they must have shown high safety, quality and efficacy in all clinical trials. In addition, there is continued monitoring of how they perform in the real world after approval to identify any rare or delayed side effects.
Efficacy
Efficacy (prounounced eh·feh·kuh·see) is the reduction in clinical signs of disease, due to vaccination, as shown in research studies carried out under controlled conditions such as randomised clinical trials.
Are there long-term unwanted impacts of COVID-19 vaccines?
There is no scientific evidence to suggest that the current COVID-19 vaccines will cause long-term problems in years to come. And in this case, where there’s been rigorous research on the topic, no news is good news.
A vaccine works by preparing your immune system to protect you against the virus without the harmful effects of the infection itself. That means it is a bit like a dress rehearsal, so that if your body is exposed to the virus it is better equipped to fight the infection. Minor side effects may occur within a few days of receiving the vaccine, as the immune system is learning how to recognise and respond to the virus. Minor side effects may include symptoms such as general tiredness, fever and muscle aches, and pain at the site of injection. Symptoms are usually mild and short-lived. It’s best to look at reliable information on the specific vaccine you’re receiving to find out more about possible side effects, and to speak to your doctor or a health professional if you have any concerns.
We know that the immune system works very quickly, so if there are serious unexpected side effects from a vaccine, these will usually occur in the first 48 hours, or at most in the first few months, not years, after vaccination.
The technologies and science behind COVID-19 vaccines have been decades in the making, so although it may seem as if scientists took only a short time to develop them they’ve actually been doing the preparation work for years. While it is true that COVID-19 mRNA vaccines are the first mRNA vaccines to be licensed for use, the development of mRNA vaccines began over three decades ago. Even before COVID-19 was detected, scientists had been studying coronaviruses—a family of viruses that includes SARS, MERS and the common cold, as well as COVID-19—and how we may be able to vaccinate against them. Research from serious infectious disease outbreaks such as MERS in 2012 and SARS in 2003 also provided a head start for COVID-19 vaccine development.

Thanks to the ongoing monitoring of billions of people around the world receiving these vaccines, even extremely rare side effects can be detected. This is how the very rare blood clotting condition, thrombosis with thrombocytopenia syndrome (TTS), was picked up. It took millions of vaccinations for the condition to be detected, when some cases were reported in people mostly within a month of receiving the AstraZeneca vaccine. There have also been rare cases of anaphylaxis and a heart inflammation condition that were linked to the Pfizer vaccine in this way. However, it must be noted that the risks of clotting and heart conditions are much, much higher with COVID-19 infection than risks associated with any current vaccine.
Can mRNA COVID-19 vaccines alter a person’s DNA?
Let’s look specifically at mRNA vaccines: could the particles injected from vaccines alter our DNA years down the track or become absorbed into our genetic makeup?
In short, no—mRNA vaccines are very unlikely to alter your DNA in either the short or long term.
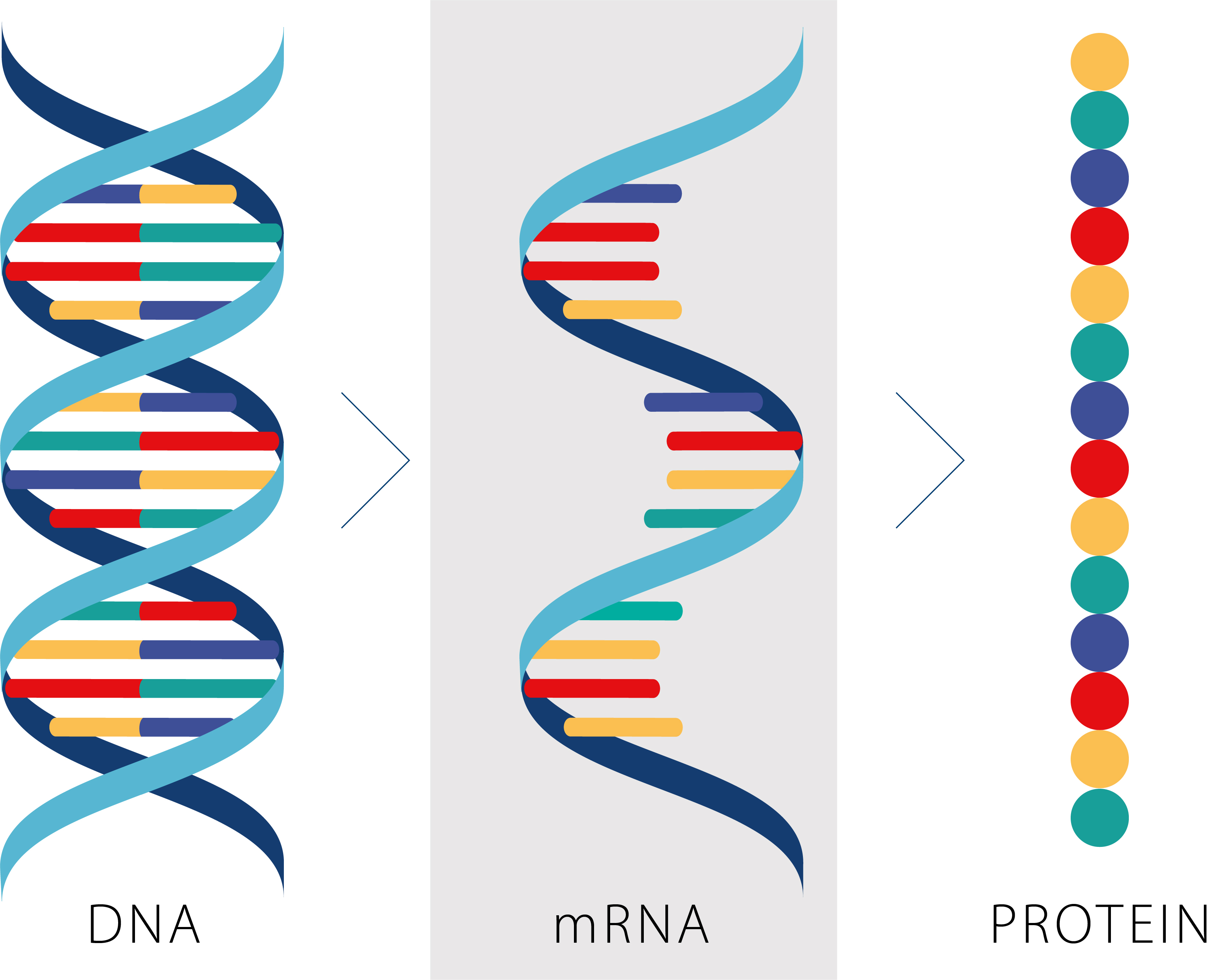
Both the Pfizer and Moderna COVID-19 vaccines use messenger-RNA (mRNA) technology. mRNA is a vital part of every living thing and acts as the translator, or messenger of information, between DNA and the cell cytoplasm where proteins are made. If you imagine DNA is a recipe book with all instructions for life, then each strand of mRNA is a photocopy of one recipe from within that book, and the protein is the final dish created by the ribosomes (the cells’ chefs). In this cooking analogy, the ribosomes read the photocopied recipe, rather than in the valuable book itself, so the book remains unaltered.
mRNA vaccines, once injected into a person’s body, deliver only part of the SARS-CoV-2 mRNA, the part that codes for the virus’s unique spike protein. Your cells’ ribosomes recognise the mRNA code and use it to create a replica of the spike protein. The spike protein of the virus won’t cause harm, as it is only one part of the virus’s outer ‘shell’—its role is to bind to other cells and to enter the body’s systems. By giving your cells’ ribosomes the instructions to make replica spike proteins, the mRNA vaccine helps your body prepare an immune response so that it can attack the spike protein when it sees it again, such as if you are exposed to COVID-19. The vaccine mRNA then rapidly degrades in your body, just as all other mRNAs do normally in any living cell. mRNA actually has a very short half-life (length of time needed for it to break down) because once its messenger job is done it is no longer needed. mRNA is naturally unstable and our cells have many different ways of degrading it. The mRNA is completely destroyed after this process, and leaves the body within a few days.
While some viruses, such as HIV, can turn their short-lived RNA photocopies into stable chapters that will insert themselves into an infected cell’s recipe book, the SARS-CoV-2 virus that causes COVID-19 can’t do that and neither can the mRNA vaccines.
The technology behind mRNA vaccines is really useful because it allows more rapid development and adaptation of vaccines and doesn’t rely on cultivating a live virus. For example, mRNA vaccines may be able to be quickly altered to better target different variants of COVID-19, if variants that make the vaccines less effective were to arise.
From years of research on vaccines, genetics and different coronaviruses, along with the massive combined international effort of monitoring and reporting on side effects of COVID-19 vaccines, we can conclude that there aren’t likely to be significant long-term side effects from COVID-19 vaccines. Whether they use mRNA or traditional vaccine technologies, safety has been a key priority. It must be noted, however, that serious long-term impacts of the actual COVID-19 infection occur in up to one in three cases of infection. So, if you are worried about your health in the long term, the best thing you can do is get vaccinated to protect yourself against COVID-19. While we can’t necessarily predict the future, we can weigh up the available evidence to make the best decision to look after ourselves and our loved ones.
This article has been reviewed by the following experts: Professor John Mattick AO FAA FTSE School of Biotechnology and Biomolecular Science, UNSW Sydney; Professor Tony Basten AO FAA FTSE Garvan Institute of Medical Research; Professor Thomas Priess John Curtin School of Medical Research, Australian National University, and Associate Professor Archa Fox School of Human Sciences, University of Western Australia. The writing of this article was supported by Academy staff: Olivia Congdon, Dr Hayley Teasdale and Alexandra Lucchetti. Published 8 November 2021.





