Tackling blood cancer
It is a special thing to be able to know that your discovery has treated cancer in hundreds, most likely thousands, of people.
Professor Andrew Roberts is a clinical haemoto-oncologist—a medical specialist and one of the Australian scientists responsible for creating a drug that treats blood cancers.
“All my research has been inspired by my patients,” Roberts says.
“As a young doctor, what really struck me was just how poor some of our treatments were for some of our sickest patients, those with leukaemias.”
The new drug that Roberts was integral in developing is called Venetoclax. Venetoclax has already proven successful in treating many cases of chronic lymphocytic leukaemia (CLL), even after other ‘standard’ therapies have all failed. CLL is relatively common in people over the age of 60, but can occur in much younger adults too. The drug can also sometimes be useful in patients with another subtype of leukaemia called acute myeloid leukaemia.
Roberts jointly won the Prime Minister’s Prize for Science and Innovation in 2019 for this discovery, and was elected a Fellow of the Australian Academy of Science in 2020.

How does Venetoclax work?
Venetoclax works by forcing ‘immortal’ cancer cells to undergo cell death.
Many leukaemias are caused, not as once thought only because there are too many cells, but by ‘super long-living’ cancer cells that do not die like normal cells, even after many cancer treatments.
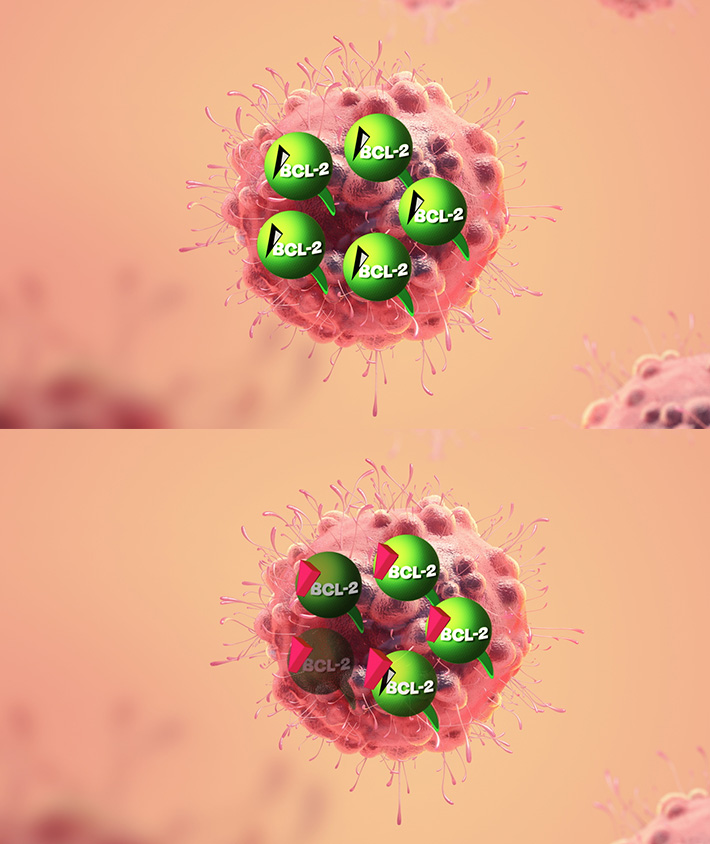
These leukaemic cells were found to have high levels of a protein called BCL-2 on the outside of mitochondria, tiny structures that generate energy within virtually all cells. BCL-2 is the key to the leukemic cell’s long life. With this knowledge, Roberts and his colleagues investigated how it was possible to disrupt this process with a drug.
They came up with a way to target BCL-2 protein using a new compound that binds with the BCL-2 and changes its function so that it doesn’t hinder the process necessary for the cancer cell to die. This allows holes to form in the outer mitochondrial membrane, and the cancer cell destroys itself.
This type of ‘programmed’ cell death, which also occurs naturally in normal cells at the end of their life, is known as apoptosis.
Once Venetoclax is in the bloodstream, the blood cancer “simply melts away”, as Roberts describes it.
“The moment that I knew that this was a true breakthrough was when the very first dose of the drug worked within 24 hours in the first patient on the very first trial in humans here in Melbourne.”
“The path to get there was long and exacting, but absolutely worth it,” Roberts says.
Apart from his lab studies, Roberts led the clinical trials process, which is rigorous testing of the drug in real patients, to ensure that the drug works and that it is safe.
They found that cancer cells are effectively killed in 80 per cent of cases, and in 20 per cent it results in total remission, meaning that even years later patients were free of cancer.
“I want to stress, it's been a team effort that’s gone on over the last 20 to 30 years,” Roberts says.
Wide-reaching impacts
Over 1000 Australians are diagnosed with chronic lymphocytic leukaemia each year and around another 900 find out they have acute myeloid leukaemia. The treatment has a huge impact on many patients and their loved ones. Venetoclax is also approved for therapeutic use in the US, promising to improve even more lives across the world.
And now, in 2020, Venetoclax is in clinical trials that are targeting other forms of blood and breast cancers. There are even suggestions that it might be used in future lung and prostate cancer treatments.
“It's an amazing feeling when it becomes clear that a patient has benefited from a drug that you've been involved in developing,” Roberts says.
“And for me, that's been incredibly rewarding. In fact, it just inspires me to keep going and try to do better.”





